NCLEX Nephrotic Syndrome
NCLEX Nephrotic Syndrome
Nephrotic syndrome is a syndrome comprising signs of nephrosis, chiefly proteinuria, hypoalbuminemia, and edema. It is a component of glomerulonephrosis, in which different degrees of proteinuria occur. Essentially, loss of protein through the kidneys (proteinuria) leads to low protein levels in the blood (hypoproteinemia including hypoalbuminemia), which causes water to be drawn into soft tissues (edema). Very low hypoalbuminemia can also cause a variety of secondary problems, such as water in the abdominal cavity (ascites), around the heart or lung (pericardial effusion, pleural effusion), high cholesterol (hence hyperlipidemia), loss of molecules regulating coagulation (hence increased risk of thrombosis). Large proteinuria is due to an increase in permeability of the filtering membrane of the kidney which normally separates the blood from the urinary space in Bowman's capsule. This is composed of the capillary walls of the glomerulus which are wrapped by highly specialized cells called podocytes. Alterations in their capacity to filter the substances transported in the blood mean that proteins but not cells pass into the urine (hence no hematuria). By contrast, in nephritic syndrome red blood cells pass through the pores, causing hematuria.Signs and Symptoms
Nephrotic syndrome is characterized by large proteinuria, hypoalbuminemia, hyperlipidemia, and edema (which is generalized and also known as anasarca or dropsy) that begins in the face. Lipiduria (lipids in urine) can also occur, but is not essential for the diagnosis of nephrotic syndrome. Hyponatremia also occurs with a low fractional sodium excretion. Hyperlipidemia is caused by two factors:- Hypoproteinemia stimulates protein synthesis in the liver, resulting in the overproduction of lipoproteins.
- Lipid catabolism is decreased due to lower levels of lipoprotein lipase, the main enzyme involved in lipoprotein breakdown. Cofactors, such as apolipoprotein C2 may also be lost by increased filtration of proteins.
- The most common sign is excess fluid in the body due to the serum hypoalbuminemia. Lower serum oncotic pressure causes fluid to accumulate in the interstitial tissues. Sodium and water retention aggravates the edema. This may take several forms:
- Puffiness around the eyes, characteristically in the morning.
- Pitting edema over the legs.
- Fluid in the pleural cavity causing pleural effusion. More commonly associated with excess fluid is pulmonary edema.
- Fluid in the peritoneal cavity causing ascites.
- Generalized edema throughout the body known as anasarca.
- Most of the patients are normotensive but hypertension (rarely) may also occur.
- Anemia (iron resistant microcytic hypochromic type) maybe present due to transferrin loss.
- Dyspnea may be present due to pleural effusion or due to diaphragmatic compression with ascites.
- Erythrocyte sedimentation rate is increased due to increased fibrinogen & other plasma contents.
- Some patients may notice foamy or frothy urine, due to a lowering of the surface tension by the severe proteinuria. Actual urinary complaints such as hematuria or oliguria are uncommon, though these are seen commonly in nephritic syndrome.
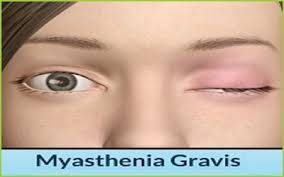
- May have features of the underlying cause, such as the rash associated with systemic lupus erythematosus, or the neuropathy associated with diabetes.
Causes
Nephrotic syndrome is usually caused by damage to the clusters of tiny blood vessels (glomeruli) of your kidneys. The glomeruli filter your blood as it passes through your kidneys, separating things your body needs from those it doesn't. Healthy glomeruli keep blood protein (mainly albumin) — which is needed to maintain the right amount of fluid in your body — from seeping into your urine. When damaged, glomeruli allow too much blood protein to leave your body, leading to nephrotic syndrome. Many diseases and conditions can cause glomerular damage and lead to nephrotic syndrome, including:- Minimal change disease. The most common cause of nephrotic syndrome in children, this disorder results in abnormal kidney function, but when the kidney tissue is examined under a microscope, it appears normal or nearly normal. The cause of the abnormal function typically can't be determined.
- Focal segmental glomerulosclerosis. Characterized by scattered scarring of some of the glomeruli, this condition may result from another disease or a genetic defect or occur for no known reason.
- Membranous nephropathy. This kidney disorder is the result of thickening membranes within the glomeruli. The exact cause of the thickening isn't known, but it's sometimes associated with other medical conditions, such as hepatitis B, malaria, lupus and cancer.
- Diabetic kidney disease. Diabetes can lead to kidney damage (diabetic nephropathy) that affects the glomeruli.
- Systemic lupus erythematosus. This chronic inflammatory disease can lead to serious kidney damage.
- Amyloidosis. This disorder occurs when substances called amyloid proteins accumulate in your organs. Amyloid buildup often affects the kidneys, damaging their filtering system.
- Blood clot in a kidney vein. Renal vein thrombosis, which occurs when a blood clot blocks a vein connected to the kidney, can cause nephrotic syndrome.
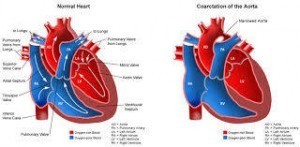
- Heart failure. Some forms of heart failure, such as constrictive pericarditis and severe right heart failure, can cause nephrotic syndrome.
Risk Factors
Factors that can increase your risk of nephrotic syndrome include:- Medical conditions that can damage your kidneys. Certain diseases and conditions increase your risk of developing nephrotic syndrome, such as diabetes, lupus, amyloidosis, minimal change disease and other kidney diseases.
- Certain medications. Examples of medications that can cause nephrotic syndrome include nonsteroidal anti-inflammatory drugs and drugs used to fight infections.
- Certain infections. Examples of infections that increase the risk of nephrotic syndrome include HIV, hepatitis B, hepatitis C and malaria.
Complications
Possible complications of nephrotic syndrome include:- Blood clots. The inability of the glomeruli to filter blood properly can lead to loss of blood proteins that help prevent clotting. This increases your risk of developing a blood clot (thrombus) in your veins.
- High blood cholesterol and elevated blood triglycerides. When the level of the protein albumin in your blood falls, your liver makes more albumin. At the same time, your liver releases more cholesterol and triglycerides.
- Poor nutrition. Loss of too much blood protein can result in malnutrition. This can lead to weight loss, but it may be masked by swelling. You may also have too few red blood cells (anemia) and low levels of vitamin D and calcium.
- High blood pressure. Damage to your glomeruli and the resulting buildup of wastes in your bloodstream (uremia) can raise your blood pressure.
- Acute kidney failure. If your kidneys lose their ability to filter blood due to damage to the glomeruli, waste products may build up quickly in your blood. If this happens, you may need emergency dialysis — an artificial means of removing extra fluids and waste from your blood — typically with an artificial kidney machine (dialyzer).
- Chronic kidney disease. Nephrotic syndrome may cause your kidneys to gradually lose their function over time. If kidney function falls low enough, you may require dialysis or a kidney transplant.
- Infections. People with nephrotic syndrome have an increased risk of infections.
Treatments
Treatment for nephrotic syndrome involves treating any underlying medical condition that may be causing your nephrotic syndrome. Your doctor may also recommend medications that may help control your signs and symptoms or treat complications of nephrotic syndrome. Medications may include:-
- Blood pressure medications
- Diuretics help control swelling by increasing your kidneys' fluid output. Diuretic medications include furosemide (Lasix) and spironolactone (Aldactone).
- Cholesterol-reducing medications. Medications called statins can help lower cholesterol levels. However, it's currently unclear whether or not cholesterol-lowering medications can specifically improve the outcomes of people with nephrotic syndrome, such as avoiding heart attacks or decreasing the risk of early death. Statins include atorvastatin (Lipitor), fluvastatin (Lescol), lovastatin (Altoprev, Mevacor), pravastatin (Pravachol), rosuvastatin (Crestor) and simvastatin (Zocor).
- Blood thinners. Medications called anticoagulants help decrease your blood's ability to clot and reduce your risk of developing blood clots. Anticoagulants include heparin or warfarin (Coumadin).
- Immune system-suppressing medications. Medications to control the immune system, such as corticosteroids, may decrease the inflammation that accompanies certain kidney disorders, such as minimal change disease.
NCLEX National Exam Courses
Overview
- Elite Reviews Offers A Variety Of Online Courses That Will More Than Adequately Help Prepare The Graduate Nurse To Pass The National Exam.
- Each Course Includes Sample Questions & The Most Current NCLEX Exam Updates.
NCLEX Free Trial
- FREE Sample Lecture & Practice Questions
- Available For 24 Hrs After Registration
- Click The Free Trial Link To Get Started - NCLEX Free Trial
How It Works
How The Course Works
- First - Purchase The Course By Clicking On The Blue Add To Cart Button - You Will Then Be Prompted To Create A User Account.
- Second - After Creating An Account, All 3 Options (90, 120, 150 Days) Will Be Listed. Select The Option You Desire And Delete The Other Two.
- Third - You Will Be Prompted To Pay For This Review Using PayPal - After Payment You Will Be Redirected Back To Your Account.
- Last - Click The Start Button Located Within Your Account To Begin The Course
- 175 Prep Questions
- Q & A With Rationales
- Alt. Format Questions
- 90 Days Availability
- Cost $75.00
- 1250+ Prep Questions
- Q & A With Rationales
- Alt. Format Questions
- 90 Days Availability
- Cost $200.00
NCLEX Practice Questions Bundle
- 1350+ Prep Questions
- Q & A With Rationales
- Alt. Format Questions
- 90 Days Availability
- Cost $225.00
NCLEX Review Course
- Option 1
- Lectures & 1250+ Questions
- Q & A With Rationales
- Alt. Format Questions
- 90 Days Availability
- Cost $275.00
- Option 2
- Lectures & 2000+ Questions
- Q & A With Rationales
- Alt. Format Questions
- 90 Days Availability
- Cost $325.00
NCLEX Review Course Bundle
- Option 3
- Lectures & 3000+ Questions
- Q & A With Rationales
- Alt. Format Questions
- 90 Days Availability
- Cost $375.00